Circulation part 1
Circulatory problems and cascade of pathology:
Circulatory problems can cause significant detriment to a patient:
If the heart is affected, e.g., during a Myocardial Infarction (MI), then it may not be pumping blood effectively around the body. If blood pressure is affected, e.g., from haemorrhage or shock, then the perfusion of organs may be compromised, causing them to fail. If there is an obstruction or clot, e.g., such as during a Stroke or a Pulmonary Embolism (PE), certain parts of the body may not be getting circulatory supply and tissues will become hypoxic and die. If the patient has blood disorders, e.g., such as sickle cell disease, this may affect the oxygen carrying capability of the blood and its’ perfusion to the rest of the body.
A wide variety of causes can affect circulation which in turn has a knock-on effect to other body systems. Organs rely on strict perfusion pressures in order to function well. If an organ isn’t getting enough perfusion, its’ cells will begin to turn hypoxic. Without oxygen, the cells will turn to an anaerobic metabolism, increasing Carbon Dioxide and acidity levels. As this continues, tissues start to die, and organ failure begins.
When an organ fails, this has a knock-on effect to other homeostatic processes within the body. Alongside this, worsening anaerobic functions of the cells produce more lactic acid and carbon dioxide, resulting in hydrogen ions and a further increase in blood acidity. Without treatment this cycle of failure continues, and more systems and organs are negatively affected. Multi-Organ Dysfunction Syndrome develops as the homeostatic balance of the body is catastrophically failing, and death is soon followed.
Assessing Circulations:
When assessing circulation, an overall view of the patient can be taken;
- Does their skin seem pale? Is it cold or are the peripheries cold to touch? Is it clammy or sweating? Pale skin, cold to touch, clamminess/sweating can be signs of poor perfusion, low Blood Pressure (BP), and/or shock.
- Is their demeanour anxious/nervous? Is their respiratory rate elevated? Do they have a reduced conscious level? All of these are signs of potential shock or circulatory issues.
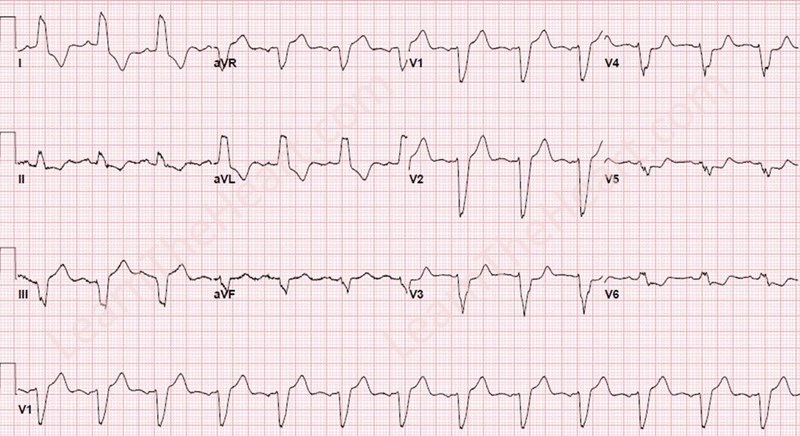
- Do they have radial pulses? Is the Heart Rate (HR) within normal parameters? Is it regular or irregular? Are both radial pulses the same? Do they feel weak, diminished, strong? Are they present at all or is it only Brachial or Carotid pulses? Tachycardia can be an indication of shock or an abnormal rhythm of the heart which may be affecting circulation. Bradycardia may also indicate an abnormality and may be affecting circulation. If the pulses feel irregular, there may be an abnormal rhythm which is causing circulatory problems. If pulses are not equal, this may indicate an issue with supply, such as a potential Aortic Aneurism or blockage. Weak or diminished pulses can give an indication of poor perfusion and BP. An Electrocardiogram (ECG) will help in identifying irregular rhythms.
- Is their Capillary Refill Time (CRT) less than 2 seconds centrally and/or peripherally? A slow central CRT may indicate poor perfusion and a bigger pathologic issue ongoing such as shock, MI, or heart failure. An isolated slow peripheral CRT may indicate poor perfusion to the limb such as a blockage or traumatic injury causing circulatory damage.
- A review of the patients’ history, signs, and symptoms will also help identify more specific potential circulatory issues, e.g., a history of unstable angina with poor coronary health, now having chest pain that won’t go, may indicate a newly developed MI.