DIB Scenario
You are working as a Paramedic, Emergency Technician crew on an Ambulance when you are called to a 57-year-old male complaining of sudden onset chest pain. He is parked in a lorry in a local industrial estate as he had just started his shift. You find the patient sat in his cab parked on the side of the road. As you open the door, he looks clammy and ashen, and you are immediately concerned. You start completing your observations whilst you get a history of the patient.
Quiz Summary
0 of 15 Questions completed
Questions:
Information
You have already completed the quiz before. Hence you can not start it again.
Quiz is loading…
You must sign in or sign up to start the quiz.
You must first complete the following:
Results
Results
0 of 15 Questions answered correctly
Your time:
Time has elapsed
You have reached 0 of 0 point(s), (0)
Earned Point(s): 0 of 0, (0)
0 Essay(s) Pending (Possible Point(s): 0)
Categories
- Not categorized 0%
-
Well done on completing the quiz. You need to score 70% or more in order to get a certificate. When you pass your quiz remember to download your certificate as proof of completing this quiz. Try and score as high as possible to show your knowledge on this subject.
- 1
- 2
- 3
- 4
- 5
- 6
- 7
- 8
- 9
- 10
- 11
- 12
- 13
- 14
- 15
- Current
- Review / Skip
- Answered
- Correct
- Incorrect
-
Question 1 of 15
1. Question
What mnemonics can you use to help with the history of pain?
CorrectIncorrect -
Question 2 of 15
2. Question
The patients’ observations are 105 HR, 26 RR, 93% Sp02, 148/82 BP, 5.2 BM, 36.6 Temp. You have also gained a brief history from your mnemonic:
Onset – 30 minutes ago, Provocation – Deep inhalation, Quality – Sharp, tightening pain, Radiating – Radiating around the chest but mainly left side, Severity – Gradual increase to 8/10 NPS, Time – Increasingly getting worse, Associated symptoms – Shortness of breath, nausea.
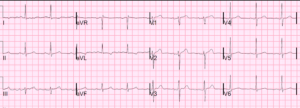
You complete a 12 lead ECG and get this result:
What is the rhythm presented?
CorrectIncorrect -
Question 3 of 15
3. Question
You are not overly concerned with the ECG presented but still consider the risks of an NSTEMI. Is aspirin still indicated in this scenario even though there is no ECG evidence of ACS?
CorrectIncorrect -
Question 4 of 15
4. Question
You look to give the patient a thorough respiratory examination as you cover your differentials. On inspection you find on deep inhalation the chest moves symmetrically but causes a lot of pain. No deformities are present on palpation. On auscultation, the left side sounds quiet compared to the right especially on the upper base. You also find hyper resonance on the left side, again on the upper base.
What diagnosis would these findings be more associated with?
CorrectIncorrect -
Question 5 of 15
5. Question
You find out the patient has pulmonary fibrosis and has been undergoing recent tests to determine the severity including a lung biopsy, making you more confident of your pneumothorax differential. The patient has no other past medical history. What treatment would you consider at this stage?
CorrectIncorrect -
Question 6 of 15
6. Question
You apply 02 but how much and what adjuncts can you use to apply it, according to JRCALC? Observations are still the same as when you complete them on arrival.
CorrectIncorrect -
Question 7 of 15
7. Question
You can use needle thoracocentesis on any patient whereby you suspect a pneumothorax developing?
CorrectIncorrect -
Question 8 of 15
8. Question
You hold off your needle thoracocentesis as there are certain inclusion criteria. What additional or worsening symptoms could you potentially see when a simple pneumothorax develops into a tension pneumothorax?
CorrectIncorrect -
Question 9 of 15
9. Question
A simple pneumothorax does not shift the mediastinal structures unlike a tension pneumothorax?
CorrectIncorrect -
Question 10 of 15
10. Question
What pain relief would be most appropriate in this scenario?
CorrectIncorrect -
Question 11 of 15
11. Question
What other differential diagnoses could be similar to pneumothorax?
CorrectIncorrect -
Question 12 of 15
12. Question
When assessing a patient’s chest with an advanced pneumothorax, you may find the effected side of the chest to either be not rising symmetrical and or hyper-inflated?
CorrectIncorrect -
Question 13 of 15
13. Question
What risk factors are associated with spontaneous pneumothorax?
CorrectIncorrect -
Question 14 of 15
14. Question
Recurrence of pneumothorax can be seen in up to what percentage of cases?
CorrectIncorrect -
Question 15 of 15
15. Question
The rupture of what structures within the lungs cause most cases of spontaneous pneumothoraxes?
CorrectIncorrect