ALS in Adults and Children part 1
Adult ALS
As discussed in the previous section, ALS cannot be started with a solo responder. Someone must be able to complete chest compressions while the other clinician carries out ALS management. The clinician may have a mechanical chest compression device available and may be able to quickly apply it to the patient, however this must not delay early defibrillation and effective CPR. Mechanical chest compression devices can be difficult to correctly place, and 2 people will likely be required to efficiently place it on the patient with minimal disruption to CPR.
When attending an adult cardiac arrest patient, the standard principles of BLS will be used at the beginning. Following placement of the defibrillation pads and starting CPR, the ALS algorithm can start. Depending on what the first witnessed rhythm is will determine treatment routes.
Shockable rhythms
There are 2 shockable cardiac arrest rhythms; Ventricular Fibrillation (VF), and pulseless Ventricular Tachycardia (pVT).
VF:
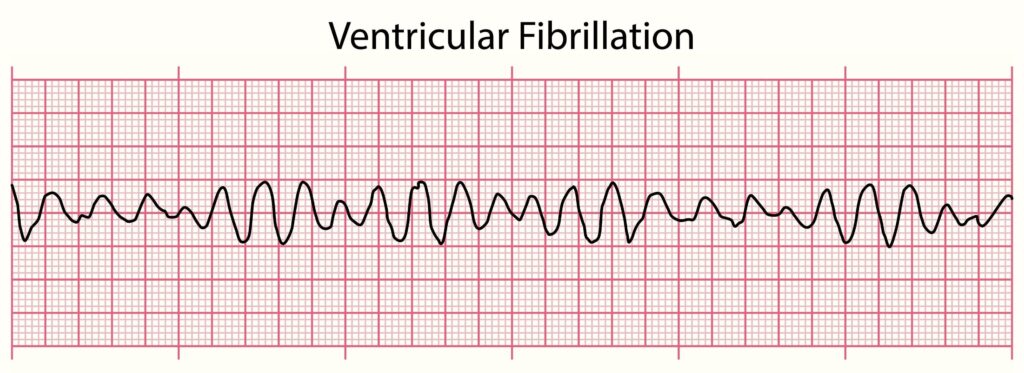
Ventricular fibrillation is a type of irregular heart rhythm. During ventricular fibrillation, lots of electrical activity fires off randomly across the ventricles. These electrical signals overcome the normal signal from the SA node, causing the ventricles to contract in a very rapid and uncoordinated manner. As a result, the heart doesn’t pump blood to the rest of the body, resulting in cardiac arrest.
Ventricular fibrillation can be caused by a disarray in electrical conduction through a problem in the heart’s electrical properties (such as in heart disease) or through a disruption of blood supply to the heart muscle (such as in a myocardial infarction).
When assessing VF on a defibrillator screen, it will look erratic with no common pattern. A simple way to remember VF is to think of ‘VF = Very Fuzzy’. There can be different degrees of VF:
Coarse VF – Where there are waves of 3 mm or more. This looks blatant on a defibrillator monitor and is often easy to spot.
Fine VF – Where the waves less than 3 mm. Where the waves are very fine, this can often be mistaken for Asystole (a flat line).
pVT:
Ventricular tachycardia is a type of irregular heart rhythm. During ventricular tachycardia, an electrical signal originates in the ventricles and causes the heart to beat faster than normal, usually 120 or more beats a minute. This electrical signal overcomes the normal signal from the SA node. Sometimes, this rapid heartbeat prevents the chambers from correctly filling with blood. As a result, the heart may not be able to pump blood, or enough blood to the body, causing a cardiac arrest.
Ventricular tachycardia occurs when the heart’s electrical system is disturbed. Reasons for this can include ischaemic heart disease, narrowing of blood vessels in the heart, structural heart disease, abnormalities in the heart valves, side effects of certain medications, electrolytes imbalances, and more.
Defibrillation is only indicated in pulseless VT. Prior to shocking a patient with VT, a quick pulse check must be made to ensure there is no pulse present. If a pulse is present, then the VT arrhythmia can pump blood around the body which will provide some level of perfusion. Defibrillating this may cause the rhythm to change to a pulseless one.
When assessing pVT on a defibrillator screen, it will look wide with a common pattern. A simple way to remember VT is to think of ‘VT = Very Tidy’. There can be other arrhythmias which result in tachycardia of the heart. To differentiate them from VT, look at the width of the QRS structure. If it is wide (greater than 120 m/s), with no P waves, this indicates its’ ventricular origin.